- Home >> ALL News >> Highlights
Mesenchymal Stem Cells Cure Autoimmune Diseases Through IGF-2-altered Metabolism in Macrophages
Mesenchymal stem cells (MSCs) are almost ubiquitous in the human body. They are among the most studied tissue stem cells because they are easily accessible and can be expanded in culture dishes. Importantly, MSCs, owing to their strong abilities to regulate immune responses, hold a great promise for the treatment of various immune disorders.
Previous studies have demonstrated that the immunoregulatory properties of MSCs are not intrinsic (Cell Stem Cell. 2008; 2:141-150), rather tightly regulated by local tissue environment (Nature Immunology. 2014; 15:1009-1016). MSCs in general are thought to enable damaged tissues to form a balanced inflammatory and regenerative microenvironment in the presence of vigorous inflammation. However, understanding of how MSCs regulate tissue microenvironment and thereby exert therapeutic effects is very limited.
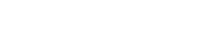
The latest work directed by Prof. SHI Yufang & Prof. WANG Ying from Shanghai Institute of Nutrition and Health, Chinese Academy of Sciences, published online on Feb. 7th, 2019 in Cell Metabolism adds exciting new information to this fast evolving field. The research findings entitled “IGF-2 Preprograms Maturing Macrophages to Acquire Oxidative Phosphorylation-Dependent Anti-inflammatory Properties” (DOI: 10.1016/j.cmet.2019.01.006) demonstrate that a low oxygen culture condition could enhance the therapeutic effects of MSCs on autoimmune diseases by up-regulating the secretion of insulin like growth factor-2 (IGF-2). The role of IGF-2 was demonstrated by genetic knockdown, specific antibody neutralization and direct administration of IGF-2 in experimental autoimmune encephalomyelitis, a mouse model of multiple sclerosis. IGF-2 was found to induce a population of PD-L1high macrophages, which in turn promote the differentiation of immunosuppressive Tregs. This effect of IGF-2 was found to be exerted through metabolically preprogramming maturing macrophages to commit oxidative phosphorylation (OXPHOS). Blockade of OXPHOS by oligomycin could diminish the therapeutic effect of IGF-2.
This study thus reveals a hitherto unappreciated mechanism of MSC-mediated therapy and provides a novel strategy for targeting macrophages in managing autoimmune disorders.
Ph.D. students DU Liming and LIN Liangyu are the co-first authors of this publication. The study was supported by grants from the National Key R&D Program of China, Chinese Academy of Sciences, National Natural Science Foundation of China, Suzhou Science and Technology Program, and Department of Science and Technology of Jiangsu Province.
Figure Legend: Low oxygen conditioned MSC metabolically reprogrammed maturing macrophages to highly express PD-L1 through production IGF-2. IGF-2- preprogrammed macrophages can promote Treg differentiation and notably inhibit autoimmune disease.
(Image by Prof. SHI Yufang and Prof. WANG Ying's Group)
Media Contact:
WANG Jin (Ms.)
Shanghai Institute of Nutrition and Health,
Chinese Academy of Sciences
Email: sibssc@sibs.ac.cn