Researchers Identify Novel Mechanism of Insulin Resistance via CREBZF-mediated Adipose Tissue Macrophage Activation
A research team led by Prof. LI Yu from the Shanghai Institute of Nutrition and Health (SINH) of the Chinese Academy of Sciences (CAS), in collaboration with Prof. ZHANG Chunxiang from the Southwest Medical University, identified a novel mechanism for CREB/ATF bZIP transcription factor (CREBZF) in chronic inflammatory responses to potentiate insulin resistance and type 2 diabetes. Entitled "Macrophage CREBZF Orchestrates Inflammatory Response to Potentiate Insulin Resistance and Type 2 Diabetes", this study was published online in Advanced Science on Jan. 29, 2024.
Type 2 diabetes is a prevalent global health challenge, with its incidence continuing to rise. Obesity-associated chronic inflammation in adipose tissue is a critical factor in triggering insulin resistance. CREBZF plays key roles in regulating nonalcoholic fatty liver disease (NAFLD), liver fibrosis, nonalcoholic steatohepatitis (NASH) and liver tissue regeneration caused by liver injury or resection. Although CREBZF has emerged as a critical metabolic regulator, its role in immune cells and chronic inflammation remains unknown.
This study demonstrated that macrophage CREBZF acts as a novel factor in regulating adipose tissue inflammation and insulin resistance. Protein levels of CREBZF are potently induced in the macrophage in response to proinflammatory signals.
To investigate the roles of CREBZF is regulating type 2 diabetes, myeloid-specific knockout of CREBZF mice were generated. The mice fed with high-fat, high-sucrose diet showed attenuated inflammation, insulin resistance and glycaemia.
Mechanistically, macrophage CREBZF promotes NF-κB signaling by competitively inhibiting the binding of IκBα to p65, which leads to enhanced transcription of proinflammatory genes.
Additionally, researchers identified bromocriptine as a small molecule inhibitor of CREBZF in macrophages, which is sufficient to suppress diet-induced proinflammatory phenotypes and improve metabolic dysfunction.
Importantly, expression levels of CREBZF are increased in adipose tissue macrophages of obese humans and mice, which is correlated with proinflammation genes and insulin resistance in humans.
These findings increased the understanding of molecular mechanisms linking obesity-related inflammation to insulin resistance, and may offer therapeutic potential for treating hyperglycemia and type 2 diabetes.
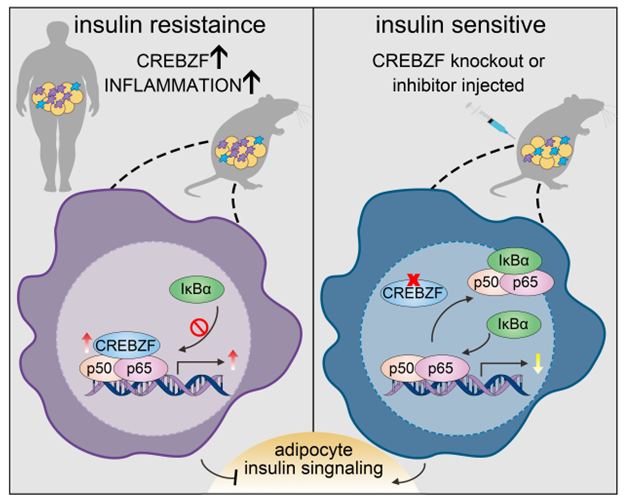
The proposed model for macrophage CREBZF in regulating adipose tissue inflammation and insulin resistance.
(Image provided by Prof. LI Yu’s group)
Media Contact:
WANG Jin
Shanghai Institute of Nutrition and Health,
Chinese Academy of Sciences
Email: wangjin01@sinh.ac.cn
Web: http://english.sinh.cas.cn/