Researchers Reveal Function and Mechanism of Deubiquitinase USP1 in Relapsed/Refractory B Cell Lymphoma
A recent study published online in Leukemia sheds light on the role and mechanisms of deubiquitinase USP1 in relapsed/refractory B cell lymphoma. The research was performed by Dr. WANG Lan’s group from Shanghai Institute of Nutrition and Health(SINH) of the Chinese Academy of Sciences and Dr. ZHANG Qun-ling, chief physician from Fudan University Cancer Hospital. Dr. WANG’s lab illustrated the key role of USP1 in rituximab/chemotherapy resistant B-cell lymphoma, providing a novel therapeutic strategy for rituximab/chemotherapy resistant DLBCL.
Lymphoma is a type of malignant tumor originating from lymphocytes and is divided into Hodgkin's lymphoma (HL) and non-Hodgkin's lymphoma (NHL). Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of lymphoma, accounting for 30-35% of NHL. In recent years, 6-8 cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone) have become the standard treatment for DLBCL, and a good efficacy of the R-CHOP regimen has been achieved. However, some patients with poor prognosis features of DLBCL remain resistant to therapy or relapse after short-term remission. It is therefore important to identify markers associated with the prognosis of DLBCL patients and the efficacy of the R-CHOP regimen, which will ultimately aid in the exploration of new targeted therapies for rituximab/chemotherapy resistant DLBCL.
To elucidate the potential role of USP1 in DLBCL, researchers detected the expression of USP1 by using immunohistochemical (IHC) analysis in 106 newly diagnosed DLBCL samples and 16 normal lymph node tissue samples. Clinical analysis showed that Ubiquitin-specific protease 1 (USP1) was highly expressed in the relapsed/refractory diffuse large B-cell lymphoma patients and its high expression predicted poor prognosis. Researchers hypothesized that USP1 could be a potential therapeutic target for the treatment of relapsed/refractory DLBCL patients and investigated the role of USP1 in DLBCL. In this study, knocking down USP1 in DLBCL cells inhibited cell proliferation, induced cell cycle arrest, stimulated autophagy, and demonstrated therapeutic effects in a xenograft mouse model of the relapsed/refractory DLBCL. Interestingly, they found that USP1 interacts with MAX and maintains the stability of the MAX/MYC heterodimer, thereby regulating the transcription of MYC target genes. Pimozide, a specific inhibitor of USP1, could significantly suppress cell proliferation, block cell cycle, increase cell autophagy and retard the growth of lymphoma in the RL-4RH cells or patient-derived xenograft (PDX) mouse model. In addition, pimozide is synergetic with chemotherapeutics such as etoposide, both in vitro and in vivo.
This study suggests that inhibition of USP1 reverses the chemotherapy resistance in relapsed/refractory B Cell Lymphoma by destabilizing MAX and MYC. These findings suggest that USP1 has an important function in relapsed/refractory DLBCL and may be a potential target for clinical therapy.
This work entitled “Inhibition of USP1 reverses the chemotherapy resistance through destabilization of MAX in the relapsed/refractory B cell lymphoma” was published online in Leukemia on Nov. 9th, 2022. It was sponsored by National Natural Science Foundation of China, Ministry of Science and Technology, Program of Shanghai Academic/Technology Research Leader, etc.
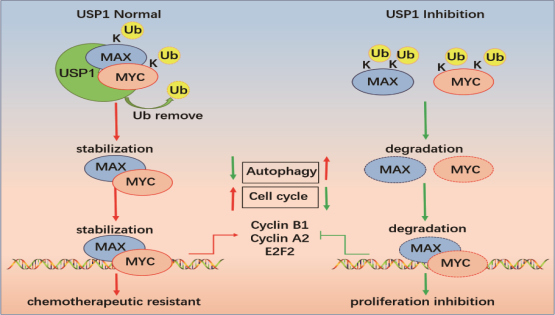
Schematic diagram of functions and molecular mechanisms of USP1 in DLBCL. (Image provided by Dr. WANG’s team)
Media Contact:
WANG Jin
Shanghai Institute of Nutrition and Health,
Chinese Academy of Sciences
Email: wangjin01@sinh.ac.cn
Web: http://english.sinh.cas.cn/